Glucocil is an over-the-counter dietary supplement that calls itself to be the “total blood sugar optimizer.” If you have Type 2 diabetes then you may have heard of Glucocil and its claims to control blood sugar.
But what exactly is it? And how does it work? We take a quick look at Glucocil and why people use it to treat diabetes.
What Glucocil Claims To Do
Made by Neuliven Health, Glucocil is marketed as the “total blood sugar optimizer.” It’s a dietary supplement for adults over 18 but not recommended if you’re pregnant or nursing.
According to Glucocil.com, it targets “3 essentials for normal blood sugar:” reducing sugar from being absorbed, reducing the liver’s sugar production, and increasing the use of sugar for energy.
It also boasts benefits of:
- Promoting healthy blood sugar levels
- Promotes heart, blood vessel & circulatory health
- Promotes healthy weight loss
- Reduces absorption of sugars and other carbohydrates
- Promotes healthy energy
Glucocil Ingredients

Glucocil contains 14 ingredients including vitamins and minerals that you’ve heard of like D3, B1, B6, B12 and Chromium picolinate.
It also has a proprietary “blood glucose management blend” that includes:
- Mulberry leaf extract
- Phellodendron extract (Berberine)
- Alpha lipoic acid
- Gymnema sylvestre extract
- Veld grape extract
- Banaba leaf extract
- Inlulina (cissus sicyoides leaf)
- Cinnamon bark powder
The ingredients in their special blend have some benefits or functions in controlling blood glucose level. But two ingredients – alpha lipoic acid (ALA) and berberine – are noteworthy compounds that we take a closer look at.
Alpha Lipoic Acid (ALA)
ALA is a naturally occurring fatty acid found in foods and created by the body. It’s an antioxidant that helps regulate or control “free radicals.”
When cells create energy from glucose and oxygen, a byproduct is created called reactive oxygen species or “free radicals.”
These free radicals are unstable molecules that can cause oxidative stress and can lead to cell damage.
ALA is known to be a powerful antioxidant that can counter many free radicals. And ALA can even create other antioxidant substances like Vitamin C and E.
ALA and insulin sensitivity
Because antioxidants help prevent cell damage, ALA and its antioxidant properties have been shown to reverse nerve damage.
Nerve damage (neuropathy) is a microvascular disease that is commonly associated with diabetes.
Chronically high blood glucose levels – a main factor for being diagnosed with diabetes – can lead to poor blood circulation and eventually damage blood vessels.
Examples includes diabetic eye disease and kidney disease which occur due the small blood vessels to these organs being damaged due to high blood sugar levels.
ALA can also improve weight
Studies have also shown that ALA can also help with weight loss. This review of clinical trials of ALA supplementing found decreases in body weight and this review saw reductions in weight and BMI.
The reason for this could be because ALA is known to increase AMPK (AMP-activated protein kinase) activity. AMPK is an enzyme that acts like a fuel sensor and is activated when cells need more energy.
Similarly, increased AMPK activity by ALA can also increase insulin sensitivity according to this study.
Phellodendron extract (Berberine)
Phellodendron is a type of plant and has been used in traditional Chinese medicine for centuries. Berberine – one chemical found in Phellondendron – is known as a potent supplement to reduce blood sugar in people with Type 2 diabetes.
This study on berberine treatment found significant reductions in Hemoglobin A1C, fasting blood glucose and post-meal blood sugar. In fact the study saw that the berberine was just as effective as metformin, which is a common and effective medication prescribed for people with diabetes.
Other Key Glucocil Ingredients
Banaba Leaf Extract
The banaba plant is found in Southeast Asia. It’s been used as a natural treatment for diabetes for years because of its hypoglycemic effects.
Banaba leaf contains corosolic acid, which has been credited for the blood sugar lowering effects of taking Banaba leaf extract.
Specifically, corosolic acid has been shown to lower blood sugar levels within 60 minutes of consumption and has antioxidant properties.
Mulberry Leaf Extract
Mulberry leaves contain many beneficial vitamins, minerals and antioxidants. And it’s why mulberry leaves have been used in natural remedies across the world for centuries.
Mulberry leaves can also help with healthier blood sugar levels. A study had participants take mulberry leaf extract with meals and saw a reduction in blood sugar increases.
This suggests that mulberry leaf extract could be a helpful mealtime supplement by minimizing blood sugar spikes.
Chromium Picolonate
Chromium is a naturally occurring earth mineral and comes in different forms.
Some forms are used in industry (like hexavalent chromium) and can be carcinogenic. And other forms – specifically trivalent chromium – is found in very small amounts in our bodies and is considered essential.
Chromium picolonate is the supplement version and is easier for the body to absorb.
While some studies have shown improved insulin sensitivity with chromium supplementing, other studies have shown no long term improvement or inconsistent results.
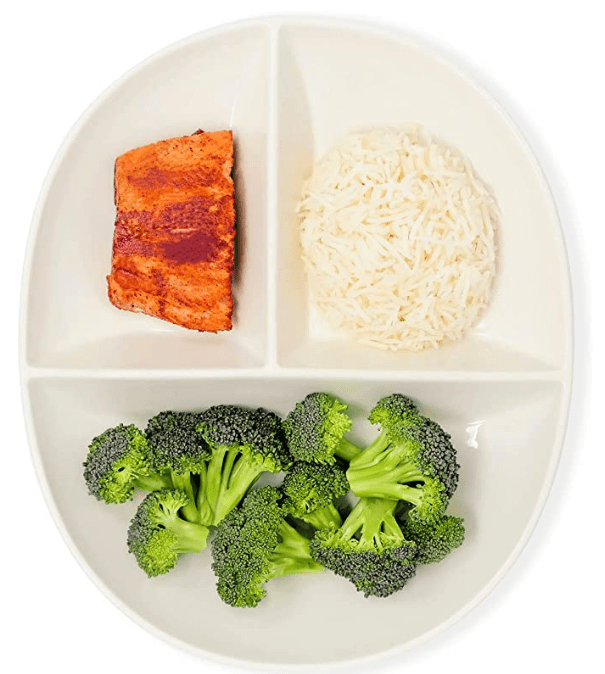
Fish Oil

Omega-3 fatty acids in fish oil is an essential nutrient and has many benefits for heart health. It’s long been established that Omega-3 can help prevent or manage heart disease, lower blood pressure and lower triglycerides.
Cissus Sicyoides
Cissus Sicyoides (princess vine) is another leaf extract and is a popular natural medicine for diabetes in Brazil.
This study found cissus sicyoides showed hypoglycemic effects on diabetic rats. However, data on its effectiveness on treating diabetes condition seem limited.
Side Effects
Every supplement and medication can have side effects. Individually, the 14 ingredients in Glucocil generally seem to be well tolerated and are likely safe for adults when taken as instructed.
But each of those ingredients can react to other medications, which is why you should talk to your doctor before taking any supplement or medication.
Summary: Does Glucocil Work?
Many of the individual ingredients in Glucocil’s proprietary blend has shown benefits for people with Type 2 diabetes – especially alpha lipoic acid and berberine.
These ingredients can help better regulate blood sugars, improve insulin sensitivity and/or have antioxidant properties to prevent nerve damage.
Some of the ingredients have also shown weight loss benefits but don’t expect it to be a weight loss diet pill.
It’s important to note that Glucocil is a dietary supplement and not an FDA-approved treatment for diabetes. There’s also very little clinical studies or Glucocil medical reviews on the products claims and effectiveness.
The product has been available for years so take the time to research customer reviews and experiences. And more importantly talk with your doctor and see if Glucocil is an option for you.