Simple guide on insulin dose adjustments when discussing with your care provider.
Insulin dose adjustments sound hard but is a must learn if you’re serious about taking control of your Type 2 diabetes. Most people with uncontrolled diabetes get little info on this, probably only when starting insulin for the first time.
But a lot of things can change blood sugar over time and taking insulin should match what your body actually needs. And learning about insulin management can reveal changes affecting blood sugar you weren’t aware of:
- Hypoglycemia or hyperglycemia: These blood sugar conditions are serious so your insulin may be the issue.
- Insulin dose not meeting needs: Prescriptions are often standardized but people’s needs are different. Your total daily insulin dose may not be giving you the results for your diabetes.
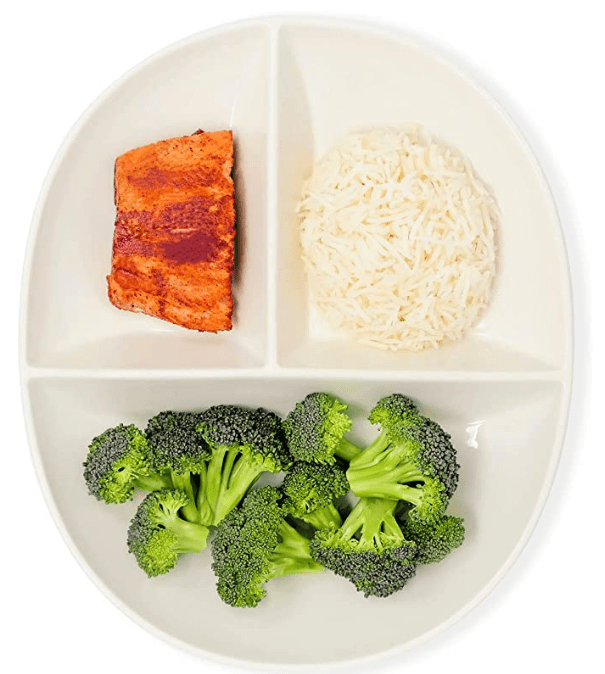
- Lifestyle changes affecting blood sugars: Eating a better diet or adding exercise can greatly improve high blood sugar and help insulin sensitivity so your dose could be giving too much insulin.
This guide includes three sections: 1) know how your insulin works, 2) check blood sugar targets and reading times, and 3) the expected insulin adjustments based on the American Diabetes Association’s (ADA) dosing guide.
You should consult your doctor or care provider’s diabetes team before making any change to your insulin dose. This guide provides helpful background when you talk to your doctor about dose adjustments to better meet your body’s current needs .
Step 1: Know How Your Insulin Works
There’s two types of insulin for controlling high blood sugar, basal and bolus. They differ in duration of blood sugar controlled and in peak times, which is when the insulin is the strongest. The peak time is also when to take a glucometer reading, usually listed as ‘x hours after meal times.’
Basal Insulin
This is a long acting insulin and lowers high blood sugar to a healthy level. Many T2 diabetes patients are prescribed a basal-only insulin regimen.
There are many basal insulins with the common generics being NPH, glargine, detemir, and degludec.
The example below charts how this long acting insulin generally keeps high blood sugar “leveled.”
Quick note on basal-only insulin regimens: if your total daily insulin dose in units is over 50% of your weight in kilograms, and your blood sugar is still not in control, you’ll likely need to start a bolus dose.
This would be better way to lower high blood sugar by adding a rapid acting insulin while being on a lower total daily insulin dose.
Bolus Insulin
This is a rapid acting insulin meant to lower or prevent high blood sugar spikes. This is usually taken before meals, sometimes called a “mealtime insulin.”
The common generic bolus insulins are regular, lispro, lispro-aabc, aspart, and glulisine.
It’s not common for T2 patients to be only on bolus. Usually, someone taking bolus insulin doses also has a basal dose.
The example below charts how this rapid acting insulin quickly lowers high blood sugar after meals.
This basic info of rapid acting insulin and long acting insulin seems minor but is important if you want to change insulin therapy to suit your lifestyle.
Wanting a lower insulin dose sounds simple but you should know how your insulin works before making changes.
Step 2: Check Target Blood Sugar and Reading Times
The glycemic target ranges below are “healthy” blood sugar levels based on the ADA 2021 Standards of Medical Care. Most care providers use these for patients but you should confirm the ranges your provider gave you.
- Pre meal (or also fasting): 80 – 130 mg/dL
- Post meal: less than 180 mg/dL
Below is when you should check blood sugar:
- Basal: measure in the AM before breakfast. But if you’re on morning NPH insulin, checking before dinner is also needed.
- Bolus: measure around 2 hours after a meal.
You can see how the insulin type, either long acting or rapid acting insulin, affects when you check blood sugar.
Important note before dosing adjustments
Any time you get a glucometer reading below 70 mg/dL, immediately consume at least 15 grams of fast-absorbing carbohydrates. After 15 mins recheck blood glucose results to see if above 70 mg/dL.
Repeat this until you get above 70 mg/dL and then eat a meal or complex carb to keep blood sugar from dipping.
Being under 70 mg/dL is hypoglycemia and can lead to hospitalization or other serious issues. So you should treat this first before working on any change to insulin doses.
Step 3: Expected Insulin Adjustments
The ADA’s 2021 Standard of Care has a guide for care providers to review a diabetes patient’s blood sugar levels and make adjustments to insulin doses (called “insulin titration”).
We summarized the ADA’s guidance below into a simple chart to show what changes to insulin doses you can expect when discussing with your doctor.
(FYI, we don’t go into detail about dosage or units of insulin because it depends on the insulin and is pretty technical. Your doctor sets the units of insulin and can explain to you if interested.)
Expected Basal Insulin Dose Adjustments
| Blood Sugars (mg/dL) | Expected Adjustments | Notes |
| Under 54 | Decrease dose by 20% | First treat low blood sugar (see above). After, check readings to see if consistently low or something caused it (changed in medication, skipped a meal, etc.). |
| 55 to 70 | Decrease dose by 10% | Same as above – first treat blood sugar and then monitor for pattern or causes. |
| 71 to 80 (or low end of target) | Monitor to see if readings consistent | If inconsistent, adjustment may not be needed. If consistent, then nearing hypoglycemia and dosage should be decreased. |
| Above 130 | Increase by 2 units every 3 days | Talk to doctor to evaluate if the change is temporary. |
Expected Bolus Insulin dose adjustments
| Blood Sugars (mg/dL) | Expected Adjustments | Notes |
| Under 180 | None | But if blood sugar is close to pre-meal target blood sugar, insulin doses may be too high. |
| Above 180 | Increase of 10% per week until on target | Before talking with doctor, check if sugar levels are consistently high or if you have high blood sugars before meals. |
This gives you an idea of expected changes to insulin doses when talking with your provider.
Final Notes to Keep in Mind
- Treat hypoglycemia first: we said this above but anytime your glucometer reading is under 70 mg/dL, consume 15 grams of carbohydrates to keep it above 70 mg/dL.
- Write down glucometer readings: give your care provider actual blood glucose results from the last 1-2 weeks. This gives them helpful, recent data to decide how to adjust your dosage.
- Total daily insulin dose: means the total doses for basal and/or bolus insulins. It’s easy to confuse total daily insulin dose as talking only about one of the insulin doses.
- Steroids impact insulin: people on steroids (ex: prednisone) usually have a fasting blood sugar within range. But after the first meal, blood sugar increases and stays high during the day. Let your provider know you’re on steroids but you can expect an insulin dose adjustment.
- “Sliding scale” or correction factor dosing: if you’re given a ‘sliding scale’ or correction factor for dosing but without a fixed dose regimen, know that it’s only for short-term dosing.
- Providers may prescribe these while in the hospital or recovering from treatment (e.g. chemotherapy) where an insulin dose adjustment was needed at that time.
- But the sliding scale or correction factor regimen is less effective than insulin doses meant for long-term blood sugar management. You should follow-up with your provider to move away from sliding scale or correction factor dosing.
Summary
Insulin dose adjustments is important for taking control of Type 2 diabetes and diabetes management overall. As you make lifestyle changes to improve high blood sugar or insulin sensitivity, you only want to inject the amount of insulin your body actually needs.
We provide a simple guide on how your insulin works, checking blood sugar against target blood sugar ranges, and what to expect for insulin dose changes talking with your provider.
We wrote an article on diabetes self-care (link here) and reviewing insulin dose is a self-care task that should be prioritized.
As always, to talk to your provider about insulin dose changes. We like to suggest that people make lifestyle changes (diet and exercise) to lower high blood sugars rather than relying only on insulin. But adjusting insulin dose is still important so you can match insulin to your body’s current needs.